Medicare provides essential health coverage for millions of Americans, including seniors and individuals with disabilities. Understanding what Medicare covers, especially when it comes to mobility products, is crucial for those in need of assistance with mobility. In this blog post, we'll delve into the intricacies of Medicare coverage for mobility products and provide clarity on how to access these vital aids.
-
Medicare Coverage Basics:
- Medicare is divided into several parts, including Part A (Hospital Insurance), Part B (Medical Insurance), Part C (Medicare Advantage), and Part D (Prescription Drug Coverage).
- Part B typically covers medically necessary durable medical equipment (DME), including certain mobility aids prescribed by a healthcare provider.
-
Eligibility for Coverage:
- To qualify for Medicare coverage of mobility products, beneficiaries must meet specific criteria, including having a doctor's prescription and demonstrating medical necessity.
- Coverage may vary depending on factors such as the type of mobility aid needed, the individual's medical condition, and whether the product is deemed medically necessary.
-
Covered Mobility Products:
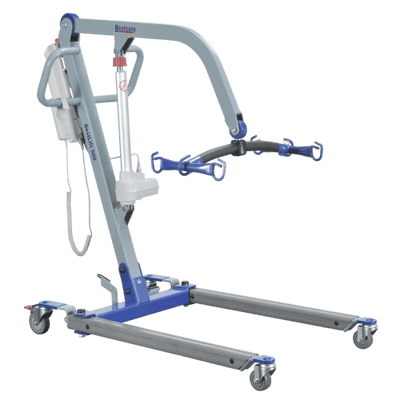
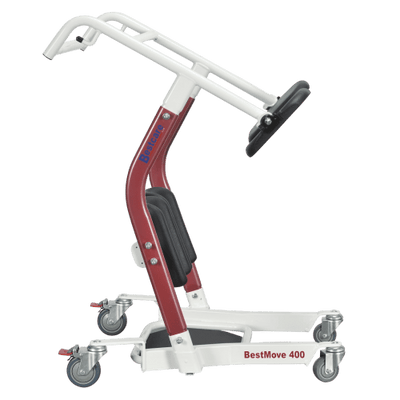
- Medicare may cover a range of mobility aids, including walkers, wheelchairs, power scooters, and canes, when prescribed by a doctor to treat a medical condition.
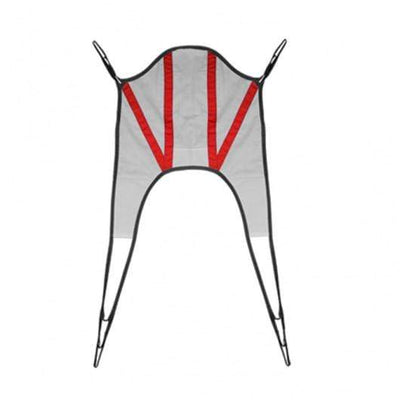
- Coverage may also extend to accessories and supplies related to mobility aids, such as wheelchair ramps, crutches, and wheelchair cushions.
-
Coverage Limitations and Requirements:
- Medicare coverage for mobility products typically requires beneficiaries to obtain the equipment from approved suppliers who accept Medicare assignment.
- Certain coverage limitations and requirements may apply, such as prior authorization, documentation of medical necessity, and compliance with Medicare's coverage criteria.
-
Alternative Coverage Options:
- In some cases, Medicare Advantage plans (Part C) may offer additional coverage for mobility products and services beyond what Original Medicare provides.
- Beneficiaries should review their plan's coverage details and consult with their plan administrator or insurance provider for information on specific coverage options and requirements.
-
How to Access Coverage:
- To access Medicare coverage for mobility products, beneficiaries should start by consulting with their healthcare provider to determine medical necessity and obtain a prescription.
- Next, they should research Medicare-approved suppliers in their area and verify coverage details, including out-of-pocket costs and billing procedures.
- Beneficiaries may also seek assistance from organizations such as State Health Insurance Assistance Programs (SHIP) or Medicare advocacy groups for guidance on navigating coverage and accessing needed mobility aids.
Navigating Medicare coverage for mobility products can be complex, but understanding the basics and knowing where to seek assistance can help beneficiaries access the vital aids they need to maintain independence and mobility. By staying informed and advocating for their healthcare needs, individuals can make the most of their Medicare benefits and live life to the fullest.